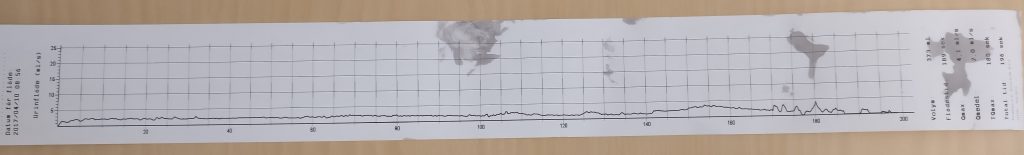
Last week I was logged in to my online medical records and noticed that I had an appointment booked with the surgeon who did my urethroplasty back in January. I hadn’t heard anything about it so I called the hospital and was told that it was a real appointment (not just a phone call). The letter about the appointment turned up the next day, saying they be doing uroflowmetry and with no other information.
So I drove up to the hospital on Tuesday and met the surgeon and was a bit surprised when he announced that he was going to try to do a quick urethrotomy while I was there. Preparation took a while (nobody could find the urethrotome), which was probably just as well since local anaesthetics take a while to take effect on me.
Since this current stricture was only about 3 cm in and very short he could get the rigid cystoscope in without any problems. It was interesting to watch him hacking away at the scar tissue on the screen. I didn’t feel a thing. He also had a quick look at the rest of the graft and seemed happy that it looked healthy and was wide enough to get the 20 Ch scope through.
Then I had time to grab a quick lunch before meeting a nurse to be instructed in how to do clean intermittent dilatation to keep the stricture open. I got some supplies but I’ll have to contact my local urology clinic for more, since I’ll be doing it daily to start with.
I’d managed to pee normally a couple of times at the hospital. There was a fair bit of blood but the local anaesthetic was still working, so it wasn’t painful. By the time I got home the anaesthetic had worn off. While I was actually peeing there was a burning sensation, which I expected and it was bearable, but afterwards I got rapidly increasing intense pain. This was really about the worst pain I’ve ever experienced, I nearly blacked out sitting on the toilet. The pain gradually faded away over a few minutes.
My husband brought some local anaesthetic gel and I took some strong painkillers but nothing seemed to help with the horrific pain every time I peed that afternoon. To make things worse my bladder was still irritated from the pressure due to the stricture so I was peeing quite often.
Then as the evening went on I started to feel worse and worse, achy and feverish. My temperature had got up to over 38°C, so my husband called a taxi and we went to the ER. I got seen fairly quickly, gave the same information to several different people and they took various samples. By around midnight they’d decided it was a post-operative infection and to keep me in but they couldn’t find a bed for me for several more hours and it was about half past three before I eventually got up to the ward.
The antibiotics seemed to start working pretty quick, so I was already feeling better yesterday and got to go home for the night. I went in this morning for the final dose of IV antibiotics and they’ve discharged me with antibiotic tablets.
So now I just have to see how I get on with the dilatation. It seems easy enough to do and the surgeon reckons that after a few months I should only need to do it once a week. I’m a bit concerned that that’ll be once a week forever but I could live with that.